Daytona Beach, FL – January 6th 2025 – Radiology Imaging Associates (RIA), a privately owned and operated radiology practice of 65 years, consisting of over 80 U.S.-based radiologists, is excited to announce the expansion of its advanced imaging services to better serve the eastern central Florida region. This expansion will be facilitated by a new division of RIA named Interventional Specialists of Florida.
Commitment to Patient Care
“At Interventional Specialists of Florida, our mission is to positively contribute to a patient’s healthcare journey by providing timely, accurate, and compassionate Interventional Radiology services. We use state of the art technology and techniques, ensuring the well-being of our patients and the trust of our clients,” said Alireza Bozorgmanesh, MD, Medical Director of ISF.
Unified Technology
Interventional Specialists of Florida will deliver advanced, minimally invasive treatments through the same proven technology that currently services a wide range of RIA clients.
Community Impact
The expansion of our radiology services represents our ongoing effort to meet the growing needs of the medical industry. By continually investing in the best interventional radiologists within a physician-centric private practice, we will continue to provide more minimally invasive surgical services to the patients we serve.
About Interventional Specialists of Florida
Interventional Specialists of Florida is a privately owned and operated interventional radiology practice uniquely positioned to succeed versus the hospital based interventional radiology offerings across the state. We are dedicated to revolutionizing the way interventional radiology is delivered by approaching each unique case with a collaborative spirit to ensure that the best solution is realized for all parties.
With a focus on excellence, precision, and price transparency, we offer a range of custom-tailored services to meet the complex needs of each patient and healthcare provider. Our cutting-edge technology and expert physician led team ensure that you receive the highest quality care and insights, allowing for improved patient outcomes and streamlined workflow. Interventional Specialists of Florida provides unparalleled Interventional services in a warm and comfortable environment, so you can rest easily knowing your interventional needs are in expert hands.
For more information, please contact:
Interventional Specialists of Florida
Phone: 386-999-ISFC
Website: isfclinic.com
Radiology Imaging Associates Announces Expansion via New Division: Select Radiology Solutions
Daytona Beach, FL – September 16, 2024 – Radiology Imaging Associates (RIA), a privately owned and operated radiology practice of 65 years, consisting of over 80 U.S.-based radiologists, is excited to announce the expansion of its advanced imaging services to better serve communities across the U.S. This expansion will be facilitated by a new division of RIA named Select Radiology Solutions.
Commitment to Patient Care
“At Select Radiology Solutions, our mission is to positively contribute to a patient’s healthcare journey by providing timely, accurate, and compassionate diagnostic imaging services. We empower healthcare providers with industry-leading turnaround times, unwavering quality, and a sustainable approach, ensuring the well-being of patients and the trust of our clients,” said Dr. Caleb Rivera, President of RIA.
Unified Technology
Select Radiology Solutions will deliver care through the same proven, AI-enabled technology stack that currently services a wide range of RIA clients.
National Impact
The expansion of our imaging services represents our ongoing effort to meet the growing needs of the radiology industry. By continually investing in the best radiologists within a physician-centric private practice, we will continue to reduce wait times and provide more comprehensive diagnostic services to the patients and clients we serve.
About Select Radiology Solutions
Select Radiology Solutions is a privately owned and operated radiology practice uniquely positioned to succeed versus the private equity radiology practice offerings across the nation. We are dedicated to revolutionizing the way diagnostic imaging is delivered by approaching each opportunity with a collaborative spirit to ensure that the best solution is realized for all parties.
With a focus on excellence, precision, and price transparency, we offer a range of sub-specialized radiology services custom-tailored to meet the complex needs of each patient and healthcare provider. Operating around the clock, 365 days a year, our team of highly trained, board-certified, U.S.-based radiologists is committed to providing accurate, dependable, and timely results whenever you need them. Our cutting-edge technology and expert team ensure that you receive the highest quality interpretations and insights, allowing for improved patient outcomes and streamlined workflow. Select Radiology Solutions provides unparalleled teleradiology services that never sleep, so you can rest easy knowing your diagnostic needs are in expert hands.
For more information, please contact:
Lisa Adams
Chief Administrative Officer
Select Radiology Solutions
Phone: 352-671-4375
Email: ladams@srsradiology.com
Website: www.srsradiology.com
The Power of Early Detection: Why Annual Mammograms Matter
As we step into October, it's essential to recognize Breast Cancer Awareness Month. At Radiology Associates, we are deeply committed to women's health and take pride in being one of Florida's highest-volume centers for 3D mammograms. Our skilled radiologists are specially trained in breast imaging, and we want to emphasize the importance of annual mammograms as a powerful tool in early breast cancer detection.
Breast cancer is a formidable adversary that affects millions of women worldwide. Early detection is crucial for successful treatment outcomes, and regular mammograms are at the forefront of this battle. The American College of Radiology (ACR) recommends that women start annual screenings at the age of 40, as these screenings can significantly increase the chances of detecting breast cancer in its earliest and most treatable stages.
Early Detection Saves Lives: Breast cancer often presents no symptoms in its early stages, making regular screenings indispensable. Mammograms can detect abnormalities such as tumors long before they can be felt, increasing survival rates dramatically.
Advanced Technology: At Radiology Associates, we employ state-of-the-art 3D mammography, also known as digital breast tomosynthesis. This advanced technology provides clearer and more detailed images, reducing the risk of false positives and ensuring early cancer detection.
Personalized Care: Our team of radiologists is dedicated to providing compassionate and personalized care. When you choose Radiology Associates for your mammogram, you are placing your health in the hands of experienced professionals who prioritize your well-being.
Peace of Mind: Regular mammograms offer peace of mind for women, allowing them to proactively manage their health. It's a simple yet powerful step towards maintaining a healthy and cancer-free life.
Community Involvement: National Breast Cancer Awareness Month is a time to unite and support one another. Radiology Associates is proud to be part of this movement, advocating for early detection and raising awareness about breast health.
We understand that taking time for your health can be challenging, but your well-being is worth it. Scheduling an annual mammogram is a small investment that can yield tremendous dividends in terms of health and peace of mind.
In conclusion, as we observe Breast Cancer Awareness Month this October, remember that early detection is key. At Radiology Associates, we are here to support you in your journey towards optimal breast health. By following the ACR's recommendation to start annual screenings at 40, you are taking a proactive step in safeguarding your future. Don't wait; schedule your mammogram today and join us in the fight against breast cancer. Together, we can make a difference in women's health and well-being.
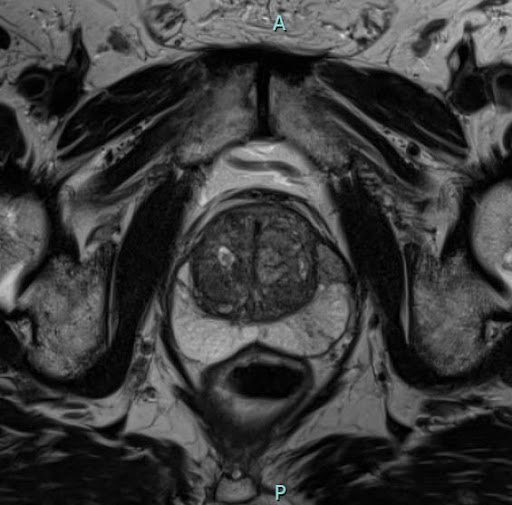
The Importance of Prostate MRI: A Message from Radiology Associates
September marks National Prostate Cancer Awareness Month, a time dedicated to shedding light on a disease that, while treatable, can have devastating consequences if not caught early. Our mission at Radiology Associates is clear: to provide accurate and timely diagnostics using state-of-the-art technology, all while treating our patients with the utmost respect and care.
Prostate cancer is the most diagnosed non-skin cancer in American men. Statistically, 1 in 9 men will be diagnosed with prostate cancer during his lifetime. While these statistics may seem alarming, they also underscore the importance of early detection and intervention. The good news is that if detected early, the 5-year relative survival rate for prostate cancer is nearly 100%.
Now, you may ask, "Why Prostate MRI?"
Magnetic Resonance Imaging (MRI) of the prostate is a non-invasive imaging technique that has revolutionized our ability to visualize, detect, and grade prostate tumors. Unlike other screening modalities, MRI offers detailed images of the prostate gland, allowing radiologists to identify lesions that might be cancerous with greater precision.
Our team at Radiology Associates is proud to share that we complete thousands of Prostate MRI exams yearly, making us one of the highest volume centers in Florida. What sets us apart is our select group of radiologists who have undergone specialized training in prostate imaging. We provide our patients and their physicians the best possible information for treatment decisions.
So, who should consider a Prostate MRI?
1. Men with elevated PSA levels: Prostate-specific antigen (PSA) is a protein produced by the prostate gland. Elevated PSA levels may indicate the presence of prostate cancer. An MRI can help confirm or rule out its presence.
2. Men with a family history: If you have a close family member – father, brother, or son – who has had prostate cancer, your risk is significantly higher.
3. Men of African descent: African-American men are more likely to develop prostate cancer and are twice as likely to die from it compared to Caucasian men.
4. Men aged 55-69: The American Urological Association recommends shared decision-making for men aged 55-69 considering PSA-based screening. If PSA levels are elevated, an MRI could be the next logical step.
5. Men who've had a previous negative biopsy but still have rising PSA levels: This is critical as traditional biopsies can sometimes miss cancer. An MRI can offer a more comprehensive look at the prostate.
Radiology Associates takes pride in being at the forefront of diagnostic imaging. But beyond technology and expertise, we are deeply committed to patient care. This September, as we shine a light on prostate cancer awareness, we urge every man to prioritize his health.
Early detection is the best weapon against prostate cancer. Let's make the choice to stay informed and proactive. Your health and future are worth it.
What is PET/CT?
One of the most advanced imaging test available to patients and radiologists is often considered to be a PET/CT scan, the combination of two different imaging technologies: positron emission tomography (PET) and computed tomography (CT). When the PET and CT scans are performed on the same machine at the same time, radiologists are able to obtain a more detailed image than either test would provide by itself.
PET is a type of nuclear medicine exam that measures the metabolic activity of the cells in body tissues, helping to visualize the biochemical changes taking place in the body. Meanwhile, CT acquires images at a variety of angles of a patient’s body, capturing organs, tissues, and bones in cross-sectional ‘slices.'
In a PET/CT scan, the PET and CT images are fused (or co-registered) together, precisely aligning the biochemical or metabolic activity seen on the PET images with the corresponding CT anatomical imaging. This technological capability provides an enhanced level of detail to radiologists, pinpointing abnormal metabolic activity and thereby enabling a more exact diagnosis.
Why is PET/CT ordered?
The use of PET/CT scanning is integral to modern healthcare. This highly specialized procedure, with an estimated two million scans performed annually, has primarily found its applications in diagnosing and monitoring cancer and brain disorders since its clinical introduction in the early 2000s.
Thanks to its multidimensional imaging capabilities, PET/CT provides precise localization of precancerous, cancerous, and certain types of diseased cells in various body parts including the skin, lungs, head and neck, breasts, ovaries, lymph nodes, testicles, thyroid, pancreas, and esophagus—even at early stages of disease.
Additionally, PET/CT scanning plays a crucial role in locating seizure activity in patients, evaluating stroke damage, and distinguishing Alzheimer's from other dementias and brain diseases. It's also used in assessing heart blood flow, identifying bone lesions, and differentiating between scars and cancers.
In the context of cancer treatment, PET/CT is instrumental in determining the stage of the disease and monitoring the effectiveness of treatments such as chemotherapy and radiation therapy.
What is injected?
As it is a nuclear medicine procedure, PET scans require the intravenous injection of a radiotracer, which is a type of radiopharmaceutical. The intravenous injection may be performed up to 90 minutes prior to the scan. Commonly used radiotracers include prostate-specific membrane antigen (PSMA), Sodium Fluoride (NaF), and brain imaging tracers like Amyvid (Florbetapir), Neuraceq (Florbetaben), and Vizamyl (Flutemetamol). These radiopharmaceuticals play a crucial role in disease diagnosis and therapy.
Preparing for a PET/CT exam
Discuss with your doctor
Before ordering a PET/CT scan, your doctor will discuss with you any existing allergies or illnesses, and review your current prescription and non-prescription medications, including vitamins and herbal supplements. If you are pregnant or nursing, this is crucial information your doctor will need to know before ordering the exam.
Recommended diet and food restrictions 24 hours before exam
For FDG PET/CT, dietary restrictions are important due to the use of glucose as the radiotracer. To prevent competing sugars from affecting the distribution of the radiopharmaceutical and subsequent image quality, avoid carbohydrate-rich foods, sugar, and caffeine in the 24 hours before the exam. Failure to do so could affect the quality of the scan and might necessitate a rescheduling.
DO NOT EAT LIST:
Carbohydrate-rich foods like bread, cereal, potatoes, rice, noodles, snack chips, or energy bars; canned foods and salad dressings that contain sugar, pickles, ketchup/barbecue sauce, or desserts or candy of any kind.
Drinks like caffeinated coffee or tea, carbonated beverages, hot chocolate, beer, wine, or alcohol.
DO EAT:
Any kind of meat or seafood, eggs, cheese, green vegetables only, and salads dressed with only oil and vinegar.
You should only drink water during this 24-hour period.
Please fast for six hours prior to the exam, consuming only water during this period.
Depending on your existing medical conditions, your doctor may give you different instructions for preparation, especially if you are diabetic.
Having the exam
When you arrive at our imaging center and have checked in, we’ll test your blood sugar and place an intravenous (IV) line in your arm. You’ll receive a radiopharmaceutical injection through the IV 60 minutes before the exam.
We’ll escort you to a special waiting room that is conducive to relaxing with minimal activity and talking. Just before the exam takes place, we’ll request that you remove any metal items from your body—this includes jewelry, hair accessories, and all clothing containing metal, and we will provide you with a locker for these items. We’ll also ask you to use the restroom to empty your bladder and to change into a provided gown before entering the PET/CT suite.
If you are claustrophobic, there is no need for concern. The PET/CT scanner is not as confining as a tubular MRI scanner; rather, it is donut-shaped and closely resembles a CT scanner. We’ll position you on your back on the scanner table in a comfortable position with a headrest.
If your doctor has prescribed medications for claustrophobia, please bring them with you and take them 45 minutes before the exam. Additionally, please arrange for someone to take you home after the exam, as it is not safe for you to drive.
The CT scan is performed first, followed by the PET scan. You’ll be required to lie still as the table you are on slowly moves through the scanner. The entire scanning process is non-invasive and painless; you won’t feel a thing.
The entire exam process takes about 20 minutes, thanks to Radiology Associates’ time-of-flight (TOF) PET/CT scanners. Our state-of-the-art scanners enhance the speed and productivity of the scan, aiming to make the exam process as comfortable as possible for patients.
TOF PET/CT scanners also acquire high-resolution imaging for all body types, including large-bodied patients, and help in enhancing image quality by reducing noise and increasing sensitivity.
After the exam
You will be asked to drink at least five glasses of water to help flush the radiotracer out of your body. The radioactive tracer emits very low radiation and will naturally diminish from your body within hours.
Your doctor will review your scans and interpret the results. They will discuss findings with you within a few days. We recommend following up with your doctor for any further questions and discussions.
Note
Safety is our utmost priority at Radiology Associates. We adhere to the highest safety standards and use state-of-the-art equipment. Our staff comprises experienced professionals who provide the highest level of care and patient-centered service.
References:
1. Radiological Society of North America (RSNA). "PET/CT". RadiologyInfo.org. Available at: https://www.radiologyinfo.org/en/info/pet (Accessed 7/4/2023.)
2. Schaart DR. "Physics and technology of time-of-flight PET detectors." Phys.Med.Biol. 2021 Apr 21;66(9). doi: 10.1088/1361-6560/abee56
3. Statistica. (2021, November). Health, Pharma & Medtech: Medical Technology section. Rate of PET examinations in the United States from 2004 to 2020 (per 1,000 population). Available at: https://www.statista.com/statistics/962337/pet-examinations-in-united-states-rate-per-one-thousand. (Accessed 7/4/2023.)
4. Suri S. "Update on time-of-flight PET imaging." J Nucl Med. 2015. 56(1):98-105. doi.org/10.2967/jnumed.114.145029.
Early Detection of Lung Cancer with LDCT Scans
At least 80% of all lung cancer cases are attributed to smoking or extensive exposure to secondhand smoke. According to the American Cancer Society estimates, there will be at least 238,340 new cases in 2023.
If you are a current smoker or stopped smoking within the past 15 years, there is something you can do to protect yourself and stay healthy: have a low-dose CT lung cancer screening exam. Similar to breast cancer screening, annual lung cancer screening provides the reassurance that you are cancer-free or identifies cancer at its earliest stages when curative treatment is most effective.
Most people don’t know when they develop lung cancer because it starts without symptoms. Only in its more advanced stages, when the cancer has started to spread to other parts of the body, do symptoms appear. These may initially include unexpected weight loss, bone or joint pain, headaches, and/or dizziness. Symptoms that may follow include a persistent dry cough, coughing up blood, unexpected exhaustion and fatigue, shortness of breath or having trouble breathing, and/or hoarseness or wheezing.
You don’t need to wait for symptoms to get checked for lung cancer. A simple exam, called low-dose CT lung cancer screening, can detect lung cancer at its earliest stages. Taking just a few minutes to perform, this highly detailed, low radiation dose imaging exam shows very fine details in the lungs with 3D clarity, pinpointing the location of suspicious lesions, and facilitating their diagnosis.
This exam can be free or nearly free-of-charge for most people who meet the high-risk profile criteria. Because of its proven effectiveness in saving lives, this exam is paid for by Medicare and by many health insurance companies.
Who is at high risk For Lung Cancer?
In 2021, the U.S. Preventive Services Task Force (USPSTF) considerably expanded its definition guidelines defining people who are at high risk of developing lung cancer.
You are now considered to be at high risk if you are 50-80 years old and have a smoking history of 20 pack years. (A pack year is equal to smoking 1 pack of cigarettes per day for 1 year, 2 packs per day for 6 months, or 1/2 pack per day for 2 years, etc.).
Race also may be a factor with respect to lung cancer susceptibility. This is only now being clinically studied, but a multi-institutional study of diagnosed lung cancer participants in the nearly 59,000-person Black Women’s Health Study published in JAMA Oncology revealed that only 34% would have met the 2021 USPSTF high-risk guidelines for lung cancer screening. So it is very important to talk with your doctor or a health cancer screening referral program healthcare staff member about your own personal history.
The proven value of annual low-dose CT lung cancer screening
When cancer is detected at an early stage, it can be treated successfully for many patients. More than 75% survive for at least five years. An LDCT screening exam is the gold standard for detecting early-stage cancers and is significantly better than a chest X-ray or a sputum cytology lab test.
The landmark clinical trial that first proved this was the National Lung Screening Trial (NLST) which was conducted from 2002 to 2010. The trial involved 53,454 high-risk individuals, current or former heavy smokers aged 55-74.
The NLST compellingly demonstrated the life-saving potential of early lung cancer screening. Participants were assigned to undergo either a Low-Dose Computed Tomography (LDCT) scan or a chest X-ray over an extended time period. The findings, published in 2011 in the New England Journal of Medicine, revealed a 20% reduction in participant mortality who underwent LDCT scans in the NLST trial.
Numerous subsequent clinical trials have proven the effectiveness of LDCT lung cancer screening. In November 2022, the findings of the longest-running lung cancer clinical trial, International Early Lung Cancer Action Program (I-ELCAP), concluded with over 87,000 participants. Of the 1,285 lung participants who had been diagnosed with early-stage lung cancers during this trial, 80% were alive after 20 years.
Should everyone have a LDCT lung cancer screening?
No. According to the USPSTF, screenings are recommended for individuals between the ages of 50 and 80 with a smoking history of at least 20 pack-years, who are currently smoking or have ceased smoking within the last 15 years.
According to a study of 5835 LCS CTs published in 2020, only about 2% of LDCT scans of high-risk individuals identify suspicious lesions. That is why high-risk profiles have been created and a lung cancer screening referral protocol established by health care providers.
Similar to a breast cancer screening, the percentage of total patients screened who have a suspicious lesion is very low. Low to begin with, this rate drops dramatically with subsequent annual scans, but it can lead to additional testing.
Much research is taking place on a worldwide basis to reduce the false-positive rate, especially with respect to the use of biomarkers and artificial intelligence (AI) software. Commercial software is being developed to assist radiologists with their diagnoses and to help identify malignant lesions from benign ones. Advances in the next few years will undoubtedly significantly reduce the false positive rate of LDCT lung scans.
If you qualify as a high-risk individual based on USPSTF guidelines, or if you think you may be at high risk for developing lung cancer, don’t wait for symptoms to appear.
Here at Radiology Associates, our subspecialized expert radiologists will interpret your thoracic CT and make recommendations to your doctor. Consult with your doctor on whether or not you should start an annual lung cancer screening. A few minutes of your time in one of our imaging centers may make all the difference.
REFERENCES
CT Colonography Screening for Early Detection of Colorectal Cancer
BACKGROUND
Colorectal cancer (CRC) is a type of cancer that originates in either the large intestine (colon) or the rectum. CRC is the 3rd most commonly diagnosed cancer in the United States, but one of the most treatable. Early detection is key to treatment, as there is a high chance of prevention by removing premalignant polyps and a possible cure if the cancer is confined to the colon.
According to a 2023 report by the American Cancer Society, there are 106,970 new cases of colon cancer and 46,050 new cases of rectal cancer in the United States each year. Individuals over 50 years old are at the highest risk of developing colorectal cancer (CRC). On average, women are diagnosed with CRC at the age of 75, while men are diagnosed at the age of 72.
However, there has been a recent rise in CRC cases in people under 50 years old, representing 11% of colon cancer cases and 15% of rectal cancer cases. This has prompted both the American Cancer Society and the United States Preventative Services Task Force (USPSTF) to recommend that routine screening for CRC begin at age 45 for all adults.
When caught early, colorectal cancer can be treated with a higher likelihood of success. Unfortunately, many cases of colon cancer are asymptomatic and go undetected until they reach a later stage. Around 60% to 70% of cases in symptomatic patients are diagnosed at an advanced stage, making them much harder to treat.
For this reason, several methods of CRC screening have been developed that are able to detect early-stage tumors while they are still highly treatable. Some of these methods include:
Colonoscopy: a thin, flexible endoscope is inserted into the rectum while the patient is under a type of anesthesia called conscious sedation. The entire colon is inspected for polyps: if a polyp is found, it can be biopsied or removed immediately.
Sigmoidoscopy: similar to a colonoscopy, a sigmoidoscope is used to inspect the rectum and only part of the colon. Not commonly used in the United States.
Stool Tests: tumors in the colon often release tiny amounts of blood and/or abnormal DNA into the fecal matter. A stool sample can be tested for these abnormalities. These tests are more expensive than CTC and have a much higher false positive rate.
CT Colonography: a radiologic imaging technology, computed tomography (aka “CT”) can be used to generate a detailed 3D digital image of the colon and the abdomen. This image can be examined by trained radiologists to detect suspicious polyps. This method does not require IV contrast or IV medications.
Screening for Colorectal Cancer
Traditionally, colonoscopy has been the mainstay of screening for colorectal cancer. Although colonoscopy is a sensitive screening test with the ability to detect very small polyps, it is also an invasive test that requires anesthesia and a downtime/recovery period of up to a week.
More recently, a technique called CT colonography (also known as “virtual colonoscopy”) has been developed as a less invasive method of CRC screening. CT colonography (CTC), is a radiographic imaging technique that uses X-rays and computer algorithms to create detailed 3D digital images of the air-filled colon and rectum. Per the findings of a 2007 study, it has been determined that CT colonoscopy is on par with traditional colonoscopy when it comes to detecting polyps greater than 1cm in size.
CT colonscopy does not require IV contrast, IV medications, or anesthesia, and you are able to drive yourself to and from your screening appointment.
You may be referred by your doctor for CT colonography if you:
Are 45 years of age (or older) and at average risk for colorectal cancer (no personal or family history of either CRC or other abnormal polyps)
Are unable to undergo traditional colonoscopy (i.e., due to technical difficulty, the procedure is contraindicated, or if you are unable to tolerate the procedure)
There are certain patients for whom CT colonography is not recommended. This may apply to you if you have:
A personal history of previous adenomas or other suspicious polyps (as these may require a biopsy for surveillance)
Active inflammatory bowel disease (active inflammation may interfere with the identification of CRC on imaging)
Family history of CRC (traditional colonoscopy is generally preferred if you are at above-average risk)
The bowel preparation for CT colonography is very similar to that required for traditional colonoscopy. As described in this article, preparation to cleanse the colon begins the evening before the appointment. A combination of laxative pills and liquid laxatives must be consumed, prompting several trips to the restroom. Although this process may seem like a chore, it is an extremely important step that enables the ability to obtain accurate, high-quality screening images of your colon.
Bowel prep pre-procedure is so essential because the residual fecal matter in the colon can either obscure existing polyps (resulting in a false negative) or may mimic a polyp that isn’t actually there (false positive). In the event that a suspicious lesion is identified on CT colonography imaging, you will be referred for follow-up with a traditional colonoscopy. This will allow for a tissue biopsy or removal of the lesion, which will be inspected under a microscope for cancerous cells.
What to expect
Before the exam
Prior to the exam, your doctor may suggest that you only consume clear liquids within the 24 hours leading up to the exam. Additionally, a laxative is recommended for adequate bowel preparation leading up to your exam. As mentioned previously, any residual stool in the colon may either obscure existing polyps or mimic polyps that do not exist.
During the exam
A thin, flexible catheter will be inserted into the rectum, and air or carbon dioxide (CO2) is introduced. This will distend the bowel and make the contours of the colon more visible on imaging. This process may cause some cramping, which is typically mild and resolves soon after the exam.
When images are ready to be taken, you will be lying on your back on the CT scanner table. You will be asked to hold your breath for approximately 30 seconds in order to minimize motion that can distort the final image. You may also be asked to repeat the images while lying on your stomach, on your side, or both. The purpose of this is to shift any residual bowel contents into different positions (due to gravity).
Conclusion
CT colonography is a valuable screening tool for colorectal cancer. With high sensitivity, convenience, and safety, CT colonography can help you take control of your health and detect colorectal cancer early.
Since it is a less invasive alternative to traditional colonoscopy, it can be useful for patients in need of early detection of cancerous and precancerous lesions. The sooner the abnormality is identified, the more quickly treatment can begin.
Radiology Associates utilizes the latest imaging technology, including state-of-the-art 3D CT scanners and specialized software, to capture detailed images of the colon and rectum. These images are then reviewed by our team of expert radiologists who are trained to identify any abnormalities or precancerous growths.
References
https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.21772
https://www.cancer.org/cancer/colon-rectal-cancer/about/key-statistics.html
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4945785/
https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening
https://www.uptodate.com/contents/screening-for-colorectal-cancer-beyond-the-basics#H4053849
What To Expect During MRI Screening for Prostate Cancer
BACKGROUND
According to the latest American Cancer Society statistics, about 1 in 8 men will be diagnosed with prostate cancer during their lifetime. Aside from skin cancer, prostate cancer is the most diagnosed cancer in men in the United States. It is more commonly detected in older men and non-Hispanic Black males, and a family history of this cancer can also heighten the likelihood of developing the condition.
While the rate of prostate cancer cases may sound alarming, it is encouraging to know that newer technologies like Prostate MRI are dramatically improving the way we view and diagnose prostate cancer.
WHO SHOULD HAVE A PROSTATE MRI?
Prostate MRI has been shown to be very helpful in the management of patients with suspected or already diagnosed prostate cancer. The most common situations to obtain an MRI of your prostate include:
Screening for prostate cancer
Staging a known prostate cancer
Following prostate cancer in patients undergoing active surveillance
SCREENING FOR PROSTATE CANCER
Screening for prostate cancer is one of the most common reasons for your doctor to order a prostate MRI. If you have a blood test showing an elevated or changing PSA value, your doctor may choose to obtain a repeat blood test later or consider other options to evaluate for prostate cancer, such as a biopsy or MRI.
You should keep in mind that an abnormal or elevated PSA value does not necessarily mean you have prostate cancer. Your PSA value can become elevated if you have a large prostate gland or if you have inflammation or an infection in the area. There is no specific PSA level below which prostate cancer can be entirely excluded.
Several major published studies over the past several years (2,3) have demonstrated that using prostate MRI may prevent around 30% of unnecessary prostate biopsies. All while helping find more “clinically significant” prostate cancer and avoiding the detection of “clinically insignificant” cancer that may not affect the patient’s health.
STAGING A KNOWN PROSTATE CANCER
If you have undergone a biopsy that revealed prostate cancer, your doctor may choose to obtain MRI prior to treatments like radiation therapy or surgery to perform “staging.” This means using MRI to evaluate the size and location of the cancer before determining if it has spread outside of the prostate “capsule” or into any adjacent organs such as the seminal vesicles.
This is important information that can affect what type of treatment is recommended, how to optimally remove or treat all the tumors, and how to determine your prognosis.
ACTIVE SURVEILLANCE
Active surveillance is sometimes referred to as the “watch and wait” treatment. This means your doctor thinks you have a “low-grade” cancer that may never need treatment or affect your health during your lifetime.
After decades of medical evidence, it is now known that many prostate cancers do not harm an individual during their lifetime if left alone. However, determining which prostate cancers can be watched versus which ones should be promptly treated can be challenging.
Prostate MRI plays a role in determining which cancers are more likely to need treatment. MRI is helpful to demonstrate whether the cancer may be a “higher-grade” or more aggressive than originally thought based on the initial biopsy. Also, we commonly perform annual follow-up MRI exams to see if the known cancer is changing in any concerning way that would prompt your doctors to initiate treatment.
WHAT TO EXPECT
Before the exam:
Prior to your appointment, you will need to answer some questions to confirm that MRI is safe for you and that you are directed to the best machine for your needs. It is important to let the scheduler know if you have any implanted medical devices or metallic foreign bodies so we can determine how best to perform your examination.
Occasionally, we require an additional imaging exam or medical document review to make sure the MRI is safe for you. You will also be asked whether you have kidney disease since the examination is ideally performed utilizing intravenous contrast. The contrast is safe for almost everyone, but if you are on dialysis, we may perform the study without contrast.
During the exam:
The examination takes between 20 to 30 minutes to complete. You will be asked to change into a medical gown that is provided and will have a final screening process prior to entering the MRI room.
It is very important that metal objects are left outside of the room unless approved, and that you answer the technologist’s questions accurately. During the examination, you will wear headphones to muffle any loud sounds from the MRI machine and will lie on your back while the technologist completes the test. Most patients find the MRI to be an easy, and sometimes relaxing, exam.
In the past, some patients with claustrophobia were unable to complete the exam. However, our Open-Bore MRI machines have the largest opening available in the industry, making it an uncommon to rare situation that someone cannot perform the exam unless the condition is severe. If you are concerned about your comfort during the test, you should inform the scheduler when making the appointment and we will make sure to allow more time to assist you during the exam.
Why choose Radiology Associates Imaging Centers for your exam?
Our state-of-the-art outpatient imaging centers have been performing Prostate MRI for over a decade. We complete thousands of these exams yearly, making us one of the highest-volume imaging centers in Florida.
Additionally, we use the most advanced MRI technology and imaging techniques to perform the study so you can find comfort in knowing that you are always getting the best examination possible.
The technical part of the MRI is only one aspect of obtaining a high-quality examination. Possibly the most important piece is the interpreting radiologist who is reviewing your images. At our centers, we use a select group of specially trained radiologists to interpret these exams to offer the best accuracy and consistency. Our radiologists are required to follow all the reporting guidelines set forth by the American College of Radiology, known as PI-RADS, which is the standard of care in prostate cancer imaging.
Written By Dr. John Gianini
References:
American Cancer Society website: https://www.cancer.org/cancer/prostate-cancer.html (Last accessed 4/7/2023)
MRI-targeted or Standard Biopsy for Prostate-Cancer Diagnosis. New England Journal of Medicine 2018; 378: 1767-1777.
Role of pre-biopsy multiparametric MRI in prostate cancer diagnosis: Evidence from the literature. Turk J Urology 2021 Feb; 47 (Supp 1): S65-S70.